Our Way Forward
After Lockdown: Perspectives from the Medical Field
The announcement from the Philippine government easing quarantine restrictions in the Philippines has left many of us with questions. “How will my life change after the lockdown? Will it be safe to go outside? How do I stay safe and protect those I love? What if a second surge occurs?” We are anxious, confused, and hungry for certainty.

The announcement from the Philippine government easing quarantine restrictions in the Philippines has left many of us with questions. “How will my life change after the lockdown? Will it be safe to go outside? How do I stay safe and protect those I love? What if a second surge occurs?” We are anxious, confused, and hungry for certainty.
The purpose of this essay is to share information from a medical perspective regarding what the COVID experience teaches us, what changes to expect and how to respond to them, and how to apply these lessons in preparing for the second surge. External factors contribute greatly to a community’s response to a pandemic. For now, this essay will focus on what we can do individually.
I am a physician whose specialty is in Infectious Diseases. I am involved in the COVID controversies as adviser of the Philippine Society for Microbiology and Infectious Diseases. Our knowledge is interim, posited from what we already know about the existing corona viruses, more than highly specific information or evidence directly related to COVID-19 . Eventually our understanding and policies will evolve and improve with changing scenarios, experience, and research.
The essay is structured as such: I will discuss what we know of the virus and the disease, testing, our response so far, and end with actionable points.
Here’s what we know. COVID – 19 has affected millions of people, killing almost 430,000 in the world (6/14/20) . The Philippines has over 25,000 confirmed cases and almost 1,000 deaths (6/14/20). The disease may not manifest any symptoms, may be mild, or may be critical and fatal. SARS-CoV 2, the virus, spreads rapidly. Respiratory droplets carry the virus from one person who coughs or sneezes to other people (usually within 1 meter of the infected) who breathe it in. The droplets also settle on surfaces like hands and inanimate objects like books, door knobs, light switches, elevator buttons and contaminate those who touch them. They survive for 3 hours in the air, 24 hours on cardboard, 48 hours on stainless steel, and 72 hours on plastic.
There is no proven specific treatment. A number of drugs including antiviral, antimalaria, anti-inflammatory medications and antibodies in the plasma of recovered patients are under investigation. There is no proven preventive drug. Vitamin C, Zinc, coconut oil, garlic, and saline washes are all unproven. There are available measures which reduce the spread of the virus such as social distancing and use of protective barriers. Disinfection kills the virus: washing hands, taking a shower or scrubbing surfaces with a detergent.
How about testing? Testing is the fad today and many companies, barangays, municipalities have joined the band wagon. A lot of misinformation, confusion, even chaos relates to its use so clarification is in order. There are 2 common types of tests: the reverse transcription polymerase chain reaction or PCR and the rapid diagnostic antibody tests or RAT.
The PCR detects genetic material, RNA, of the virus in the respiratory droplets from throat swab or respiratory secretions. A positive result is the gold standard for diagnosis of COVID-19 infection. Since dead virus may still cause a (+) result, a negative result is not required to ascertain recovery or safety. Neither is it used to gauge infectiousness. The PCR is performed in accredited hospital laboratories, takes days for results to come and costs 5 thousand pesos up.
The Rapid Diagnostic Tests (RDT, RATk) are the popular tests used all over the Philippines, a result of politics, good salesmanship, effective misinformation and poor judgment. The RDT detects antibodies, IgG and IgM in the serum. These appear 5-7 days from the onset of the illness and signify the response of the body to the virus. A {+} IgG antibody in a previously confirmed COVID 19 patient means recovery and can be used as clearance for return to work. A (-) both IgG and IgM may mean no infection up to 7 days prior to the test, not no infection at the time of the test. For other purposes, RDTs are unreliable. False {+} occur from other coronavirus infections like the common cold. False (-) occurs if done at an early stage of the disease. RDTs cannot diagnose COVID-19 disease or determine infectiousness or immunity RDTs should not be used for or self-testing, mass testing or screening. RDT kits are bought from manufacturers and tests are done in clinics, local laboratories. Results are available in hours and cost is less than 2 thousand pesos.
Where are we now? The World Health Organization (WHO) announced that COVID 19 “may never go away”. Many scientists agree that it is here to stay and like HIV, we will learn to live with it. We will not go back to 2019. We will not do the things we used to do: greet friends with kisses and hugs, attend lavish parties with hundreds of guests, cheer in jam packed basketball games, or just walk freely in and out of crowded malls. Things will look different. Public and private health measures to contain the virus and prevent a second surge shall continue. We shall undergo Quarantine in its various forms (ECQ, GCQ, MECQ, etc.) and applications.
The lifting of the ECQ to MEQ or GCQ allows the resumption of ambulatory healthcare as transformed clinical practice. In-person appointments will have to be pre-scheduled, and it will be limited. Only one companion shall accompany an elderly or disabled patient. Screening at the entrance to the healthcare facility will include questions regarding exposure and symptoms, thermal scanning, and limited inspection. Suspected sources of infection will be isolated. Distancing between patients, one way paths and minimum physical contact will be enforced. Masks, face shields, gowns and gloves; alcohol, UV lamps and air purifiers will be everywhere. Windows will be open and air conditioning turned off.
The face to face prolonged physician patient encounter will be replaced by a telemedicine conversation and video visualization of physical and laboratory findings. Only when necessary will a brief directed gloved physical examination be done. Prescription and billing will be telecommunicated.
What can we do? First, we need to take care of ourselves physically and mentally by exercising, maintaining a healthy diet, resting, and remaining hopeful. We must remember to be gentle with ourselves, taking note of situations that overwhelm us and cause us stress. Allowing ourselves moments of rest will help us stay resilient in the long term. Keeping in touch with friends and family can help us, and those around us.
Second, protect your loved ones and your community by staying home and remaining informed. Being informed means searching for accurate and updated information. Before sharing anything, we must ensure that the data we are sharing is accurate. The World Health Organization, the Center for Disease Control, and the Philippine society for Microbiology and Infectious Diseases are good sources of medical information. Keep faith that legitimate science works.
Third, support your community. Follow effective public health habits that prevent spread. Stay home whenever you can. Isolate and practice cough etiquette. Be altruistic if you have the means: share more than save. Extend concern not only for your own families, but for strangers and the larger community that you belong to. Now is not the time for discrimination against COVID patients, healthcare workers, Chinese people, foreigners or OFWs.
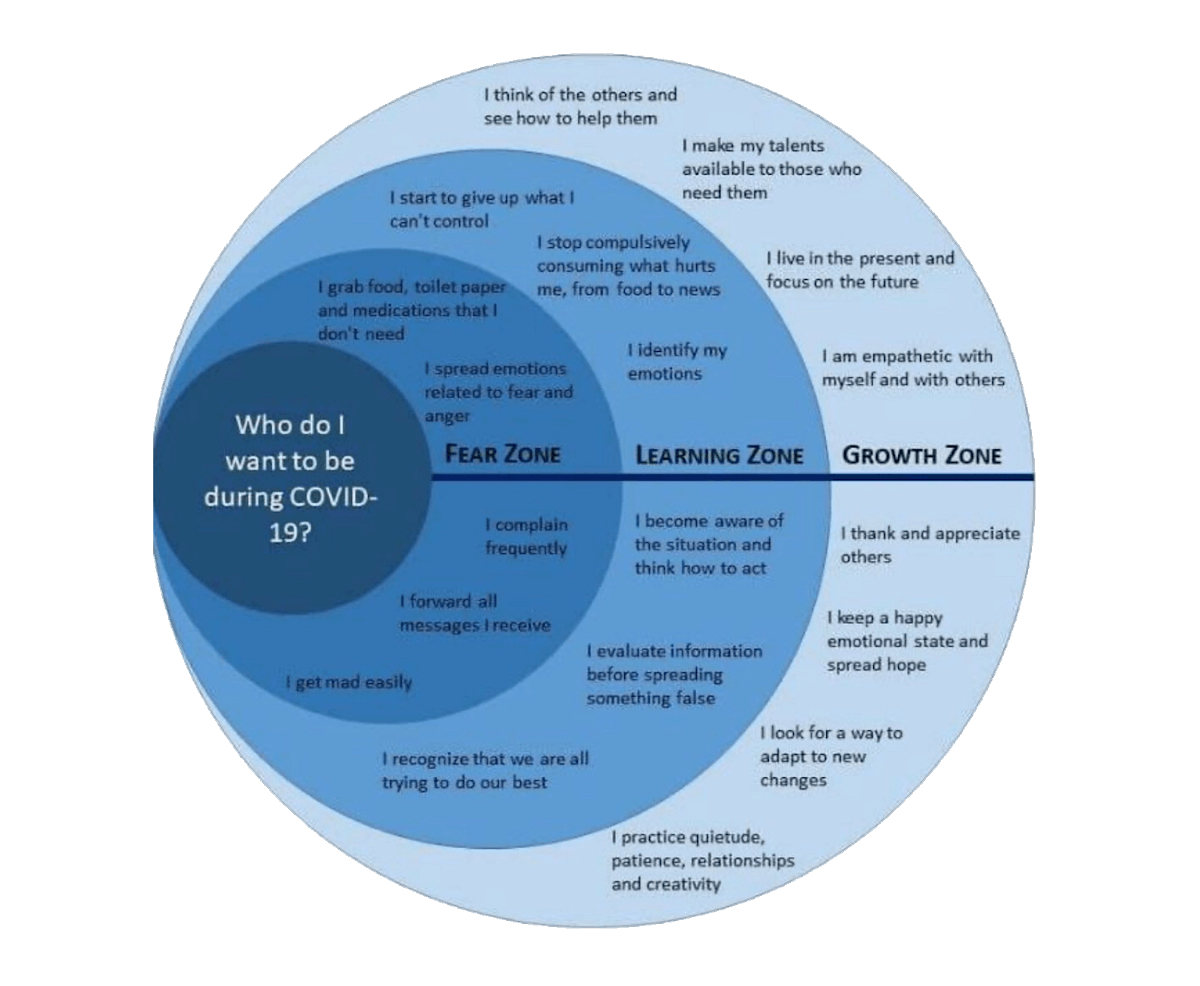
Circular graphic courtesy of Celina Canales
So, what is next? Will the curve flatten? Will a second surge occur? Will there be a new pandemic? In all honesty, we are not certain. We do know that distance, barriers, disinfection, quarantine reduce the spread of viruses. We also know that these medical mainstays are only part of the proper behavior which will determine how prepared we are to contain COVID 19 today and whatever other virus tomorrow. What we each do, how we behave, and who we want to be is our choice.